|
|
synonyms: Chronic extertional compartment syndrome, CECS, nontraumatic compartment syndrome, march gangrene, exercise-induced compartment syndrome (EICS)
CECS ICD-10
CECS ICD-9
- 729.72 nontraumatic compartment syndrome fo the lower extremity
- 958.90 Compartment syndrome unspecified
- 958.91 Traumatic compartment syndrome of upper extremity
- 958.92 Traumatic compartment syndrome of lower extremity
CECS ICD-10
- M79.A11 Nontraumatic compartment syndrome fo the right upper extremity
- M79.A12 Nontraumatic compartment syndrome fo the left upper extremity
- M79.A19 Nontraumatic compartment syndrome fo the unspecified upper extremity
- M79.A21 Nontraumatic compartment syndrome fo the right lower extremity
- M79.A22 Nontraumatic compartment syndrome fo the left lower extremity
- M79.A29 Nontraumatic compartment syndrome fo the unspecified lower extremit
CECS Etiology / Epidemiology / Natural History
- An exercise-induced increase in muscle size can result in elevated intracompartmental pressures and progress to tissue ischemia.
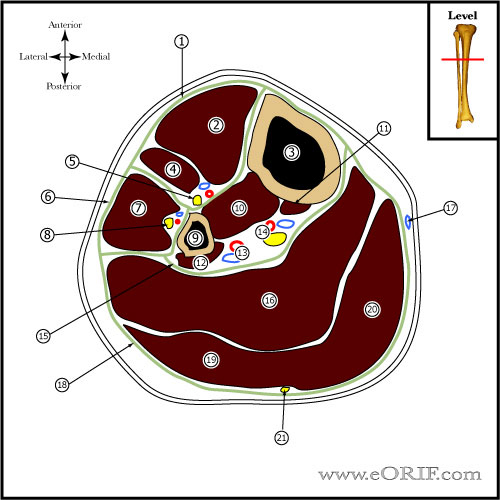
CECS Anatomy
- Leg Compartments: (1) Anterior, (2) Lateral, (3)Superficial Posterior, (4)Deep Posterior.
- Anterior Compartment (contains:Tibialis Anterior ,EHL, EDL, Peroneus tertius, Deep Peroneal nerve, and the anterior tibial vessesls)
- Lateral Compartment (contains:,Peroneus longus , Peroneus brevis, and the Superficial Peroneal nerve)
- Superficial Posterior Compartment (contains: Gastrocnemius, soleus, Plantaris, and the Sural nerve)
- Deep Posterior Compartment (contains:Popliteus, FHL, FDL, Tibialis Posterior, Tibial nerve and the posterior Tibial vessels)
CECS Clinical Evaluation
- pain after running a particular distance, may last for a few hours after finished running. Pain is usually localized to a compartment and resolves with discontinuing activity
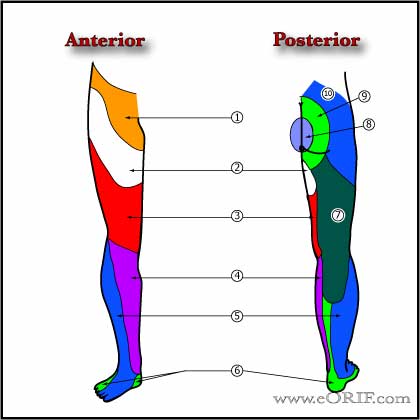
- anterior and lateral compartments most common. Has been described in shoulder, arm, forearm, hand, thigh, foot.
- 39%-46% of pts have fascial defects over the anterolateral lower leg compared with <5% in asymptomatic individuals. Defects generally 1-2cm2 in size and near the intermuscular septum between anterior and lateral compartments, often at exit of superficial peroneal nerve. Usually at junction of middle and distal thirds of leg. At rest no palpable abnormality may be apparent, but with exercise, local tenderness and swelling occur. Occasionally may have + Tinel’s sign.
- pain begins as dull ache with activity and progresses to point where activity must be stopped. Pain typically in entire affected compartment. May note transient numbness, parasthesias, weakness. Pain relieved with rest.
- Most often bilateral
- Physical exam is normal at rest; may have tenderness, fascial defect/swelling immediately following exercise.
CECS Xray / Diagnositc Tests
- A/P and Lateral of tibia indicated to evaluate for Tibial Stress Fracture.
- Diagnosed with pre- and post- exercise compartment pressure measurements. Resting pressure >15mmHg and/or a measurement taken 1 minute after exercise >30mmHg or 5 minutes after >20mmHg. (Pedowitz RA, Am J Sports Med, 1990:18:35)
- Continuous pressure monitoring during activity until pain forces subjects to stop provides higher sensitivity and specificity than measuring at 1 and 5 minutes. (Roscoe D, Am J Sports Med. 2015 Feb;43(2):392-8).
- Consider Bone Scan: Medial Tibial Stress Syndrome demonstrates diffuse moderate increased activity along posteromedial border of tibia. Stress fractures demonstrate more focal, intense often fusiform reaction. Chronic exertional compartment syndrome has normal bone scan.
CECS Classification / Treatment
- Non-op = activity modification. Only effective if pt gives up offending activity.
- Operative = fasciotomy. One incision technique, Two incision technique.
- Fasciotomy for posterior exertional compartment syndrome has lower success rate that fasciotomy for anterior compartment syndrome due high potential for inadequate release of the FDL. (Hislop M, AJSM 2003;31:770).
CECS Associated Injuries / Differential Diagnosis
- Incidence =4.5-13%
- Recurrence=7-17%; Recurrence occurs at a mean of 23.5 months post op. Potential causes of recurrence: postsurgical fibrosis/scar, iinadequate fascial release, failure to recognize involvement of other compartments, nerve compression, misdiagnosis.
- Bleeding
- Wound infection
- Nerve entrapment / Nerve injury
- Swelling
- Arterial injury
- Hematoma / hemorrhage / seroma
- Lymphocele
- DVT
CECS Follow up care
- ice/elevation 3-5 days
- immediate AROM
- crutches prn, encourage ambulation, WBAT
- full activities when tolerated usually 3-4 wks after sugery. Light activity at 2-4 wks, full activity at 4-6 wks.
- Expect 81%-100% improvement. Deep posterior compartment = 50-65% relief.
- Military: 78.2% successful outcomes; 44.7% symptoms recurrence; 27.7% unable to return to full activity; 15.7% complications after fasciotomy. (Waterman BR, JBJS 2013 95A:592)
CECS References
- Fraipont, MJ. JAAOS 2003;11:268
- Detmer DE, AJSM 1985;13:162
- Bray AW et al: Chronic exercise-induced compartment pressure elevation measured with miniaturized fluid pressure monitor. American Journal of Sports Medicine 1988;16: pp. 610-615.
- DeLee & Drez's, Orthopaedic Sports Medicine: 3e; 2009

- Aweid O, Del Buono A, Malliaras P, Iqbal H, Morrissey D, Maffulli N, Padhiar N. Systematic review and recommendations for intracompartmental pressure monitoring in diagnosing chronic exertional compartment syndrome of the leg. Clin J Sport Med. 2012 Jul;22(4):356-70. doi: 10.1097/JSM.0b013e3182580e1d.
- Pedowitz RA, Hargens AR, Mubarak SJ, Gershuni DH. Modified criteria for the objective diagnosis of chronic compartment syndrome of the leg. Am J Sports Med. 1990 Jan-Feb;18(1):35-40.
- Waterman BR, Liu J, Newcomb R, Schoenfeld AJ, Orr JD, Belmont PJ Jr. Risk factors for chronic exertional compartment syndrome in a physically active military population. Am J Sports Med. 2013 Nov;41(11):2545-9.
- Schepsis AA, Fitzgerald M, Nicoletta R. Revision surgery for exertional anterior compartment syndrome of the lower leg: technique, findings, and results. Am J Sports Med. 2005 Jul;33(7):1040-7.
|